Abstract
Background: Several novel therapeutics are being developed for AML with demonstrable effects on response rates (e.g. complete remission [CR], CR with incomplete hematologic recovery [CRi], CR with incomplete platelet recovery [CRp], overall response rate [ORR = CR+CRi/CRp]), and EFS. Improvement in EFS recently served as the basis of approval of gemtuzumab ozogamicin (GO) for the treatment of newly-diagnosed CD33-positive AML in adults (Jen et al. Clin Cancer Res 2018). The relationship between response rate, EFS, and OS in newly-diagnosed AML has not been conclusively established. Therefore, we conducted trial-level and patient-level meta-analyses of newly-diagnosed AML trials submitted to the FDA.
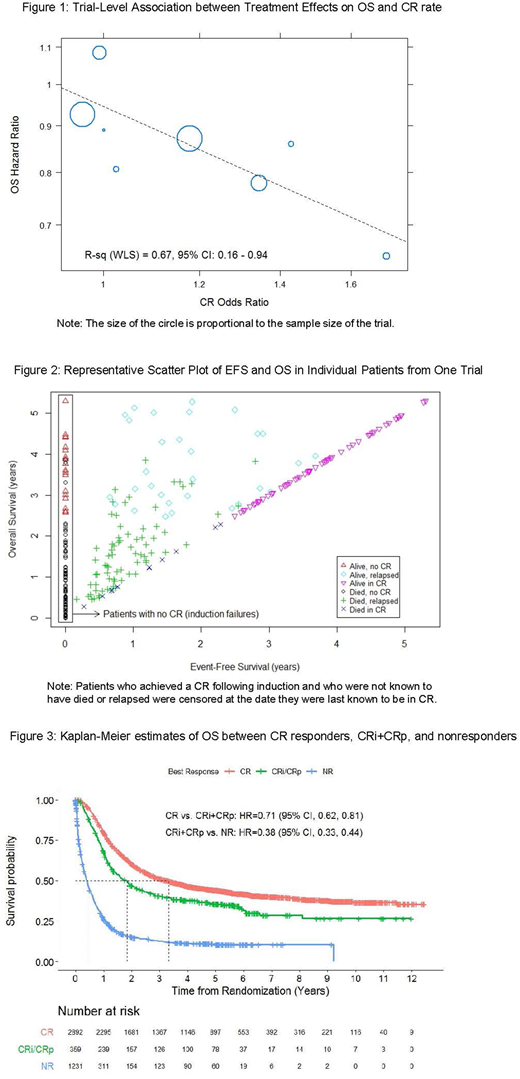
Methods: We searched for trials submitted with Biologics License or New Drug Applications for treatment of newly-diagnosed AML between 2007 and 2017. Criteria for inclusion were randomized, active-controlled, multicenter trials of intensive AML induction and consolidation chemotherapy. The estimated odd ratios (OR - ratio of odds of response in treatment to odds of response in controls) of CR and ORR and hazard ratios (HR - ratio of hazard of treatment versus control) for EFS and OS were calculated for each study. EFS was defined as time from randomization to treatment failure (defined as date of randomization for patients who failed to achieve CR following induction), disease relapse following CR, or death. Associations between treatment effects at the trial-level were evaluated using weighted least square (WLS) regression analyses on the log-scale (weighted by sample size of each randomized comparison). Coefficient of determination (R2) and 95% confidence interval (CI) were calculated to measure the strength of associations. Individual patient data for OS were plotted against EFS to explore their relationship. An exploratory patient-level responder analysis was performed to compare OS between responders and non-responders, regardless of treatment assignment in the pooled dataset. We estimated HRs of OS from Cox proportional hazards models. OS estimates by response were obtained based on the Kaplan-Meier method.
Results: We identified 8 trials with a total of 4482 patients and 3 experimental agents (GO, n=5; [daunorubicin and cytarabine] liposome injection, n=2; midostaurin, n=1) for treatment of newly-diagnosed AML. Two trials tested therapy in defined patient populations (FLT3 mutant = 1 and secondary AML = 1). The association between OS HR and CR OR at the trial-level was moderate (R2 = 0.67, 95% CI: 0.16 - 0.94; Figure 1), whereas the association between OS HR and ORR OR was weak (R2 = 0.43, 95% CI: 0.03 - 0.98). For the OS vs. EFS HR analysis, a weaker than expected association was observed (data to be presented at the meeting). Individual patient level data scatter plots suggested that one possible reason for the lack of a strong association between EFS and OS was that early failures and relapses did not always result in worse OS (Figure 2). In the patient-level responder analysis, patients who achieved a CR response had better OS compared with CRi+CRp response and no response (Figure 3).
Conclusions: On a trial level, the meta-analysis of randomized, active-controlled trials in newly-diagnosed AML suggests a moderate association between OS and CR rate, but not ORR. A strong association between EFS and OS is not established and may be confounded by improvements in salvage therapy, supportive care, hematopoietic stem cell transplantation, and/or differing censoring across trials. A patient-level responder analysis showed that CR responders have better OS compared with CRi+CRp responders and nonresponders. While our results are limited by the number of trials, they suggest that CR remains the response endpoint associated with greatest long-term benefit and that EFS, while clinically meaningful, is not a surrogate for OS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.